Advertisement
Supported by
Why Testing Still Matters
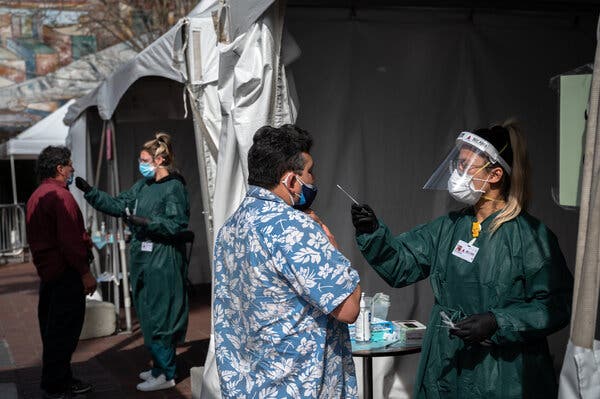
With case numbers still high, coronavirus testing remains essential, experts say, but the goals and approach will change as vaccines roll out.

Last May, the city of Los Angeles turned a fabled baseball park into a mass testing site for the coronavirus. At its peak, Dodger Stadium was testing 16,000 people a day for the virus, making it the biggest testing site in the world, said Dr. Clemens Hong, who oversees coronavirus testing in Los Angeles County.
But in January, the city pivoted, converting the stadium into an enormous, drive-through vaccination site. Local demand for coronavirus testing has plummeted, Dr. Hong said. He said that he saw the evidence firsthand recently when he visited a community hospital: “The testing site had three people and the vaccine site had a line around the block.”
Los Angeles is not an anomaly. Across the nation, attention has largely shifted from testing to vaccination. The United States is now conducting an average of 1.3 million coronavirus tests a day, down from a peak of 2 million a day in mid-January, according to data provided by the Johns Hopkins Coronavirus Resource Center.
In some ways, the decline is good news, and can be attributed, in part, to falling case numbers and the increasing pace of vaccination. But the drop-off also worries many public health experts, who note that the prevalence of Covid-19 remains stubbornly high. More than 50,000 new cases and 1,000 deaths are being tallied every day and just 14 percent of Americans are fully vaccinated.
“We are very much worried about resurgence,” said Jennifer Nuzzo, an epidemiologist at Johns Hopkins University. “Everybody mentally moved on to vaccines. Obviously, vaccines are quite important. But as long as the majority of us are not protected, then testing remains essential.”
The $ 1.9 trillion stimulus package signed into law this month includes $ 47.8 billion earmarked for testing, tracing and monitoring the virus.
But as society begins to reopen and vaccines roll out more widely, testing strategies are evolving. Here are four reasons that testing still matters, and how officials see the next months, and years, playing out.
Diagnosing people who are sick
Case numbers remain high, and clinicians still need to identify individuals who have contracted the virus so that these people can receive proper treatment and care. The gold standard for diagnosing Covid-19 is the polymerase chain reaction, or P.C.R., test, which can identify even small traces of genetic material from the coronavirus.
This kind of testing will be needed as long as there are Covid-19 cases, but as the disease becomes less common, diagnostic testing is likely to become less centralized.
“The game has changed a little bit,” Dr. Hong said. “Before, we just had infection popping up everywhere, and we just needed broad, blanket testing access. Now we need to be much more targeted.”
Diagnostic testing is shifting from large, government-run sites to smaller, more distributed sites that are spread across local communities, Dr. Hong said. Ultimately, when vaccination rates are high enough and cases are low enough, dedicated testing sites will not be needed at all. “Then we just return testing to the health care system,” he said, and coronavirus tests will simply be one of many options on the menu at the doctor’s office.
Slowing the spread
Testing is important not just for identifying individual patients who need treatment but also for public health. When the system is working, a timely Covid-19 diagnosis is what triggers contact tracing and quarantining and can stop virus transmission in its tracks.
“The vaccine — marvelous, miraculous as it is — is not in and of itself going to contain this pandemic,” said A. David Paltiel, a professor of health policy and management at Yale School of Public Health.
Slowing transmission means fewer people will get sick but it also gives the virus fewer opportunities to mutate. And that reduces the odds that dangerous new variants — some of which may be able to evade vaccine-induced immunity — will emerge.
Keeping community spread low will help give vaccines “a fighting chance,” Dr. Paltiel said. “The less work we give the vaccine to do, the better.”
As schools and offices reopen, routine screening of asymptomatic people will help minimize viral spread. These screening programs are now beginning to ramp up. Many will rely on rapid antigen tests, which are less sensitive than P.C.R. tests but are cheaper and can return results in 15 minutes. (Antigens are molecules, like the well-known spike protein, that are present on the surface of the coronavirus and trigger the immune system to produce antibodies.) When antigen tests are used routinely and frequently, they can be effective in identifying infectious individuals and reducing viral transmission, several analyses suggest.
As vaccination rates increase, these screening programs may become more targeted. If 70 percent to 80 percent of Americans are vaccinated, the prevalence of Covid-19 plummets, and outbreaks are not emerging in group settings, then it may be possible to ease up on widespread screening, said Dr. Mary K. Hayden, an infectious disease specialist at Rush University Medical Center in Chicago. “Then, yes, I think we could relax surveillance testing,” she said before adding, “But it’s a lot of ‘ifs.’”
Frequently Asked Questions About the New Stimulus Package
The stimulus payments would be $ 1,400 for most recipients. Those who are eligible would also receive an identical payment for each of their children. To qualify for the full $ 1,400, a single person would need an adjusted gross income of $ 75,000 or below. For heads of household, adjusted gross income would need to be $ 112,500 or below, and for married couples filing jointly that number would need to be $ 150,000 or below. To be eligible for a payment, a person must have a Social Security number. Read more.
Buying insurance through the government program known as COBRA would temporarily become a lot cheaper. COBRA, for the Consolidated Omnibus Budget Reconciliation Act, generally lets someone who loses a job buy coverage via the former employer. But it’s expensive: Under normal circumstances, a person may have to pay at least 102 percent of the cost of the premium. Under the relief bill, the government would pay the entire COBRA premium from April 1 through Sept. 30. A person who qualified for new, employer-based health insurance someplace else before Sept. 30 would lose eligibility for the no-cost coverage. And someone who left a job voluntarily would not be eligible, either. Read more
This credit, which helps working families offset the cost of care for children under 13 and other dependents, would be significantly expanded for a single year. More people would be eligible, and many recipients would get a bigger break. The bill would also make the credit fully refundable, which means you could collect the money as a refund even if your tax bill was zero. “That will be helpful to people at the lower end” of the income scale, said Mark Luscombe, principal federal tax analyst at Wolters Kluwer Tax & Accounting. Read more.
There would be a big one for people who already have debt. You wouldn’t have to pay income taxes on forgiven debt if you qualify for loan forgiveness or cancellation — for example, if you’ve been in an income-driven repayment plan for the requisite number of years, if your school defrauded you or if Congress or the president wipes away $ 10,000 of debt for large numbers of people. This would be the case for debt forgiven between Jan. 1, 2021, and the end of 2025. Read more.
The bill would provide billions of dollars in rental and utility assistance to people who are struggling and in danger of being evicted from their homes. About $ 27 billion would go toward emergency rental assistance. The vast majority of it would replenish the so-called Coronavirus Relief Fund, created by the CARES Act and distributed through state, local and tribal governments, according to the National Low Income Housing Coalition. That’s on top of the $ 25 billion in assistance provided by the relief package passed in December. To receive financial assistance — which could be used for rent, utilities and other housing expenses — households would have to meet several conditions. Household income could not exceed 80 percent of the area median income, at least one household member must be at risk of homelessness or housing instability, and individuals would have to qualify for unemployment benefits or have experienced financial hardship (directly or indirectly) because of the pandemic. Assistance could be provided for up to 18 months, according to the National Low Income Housing Coalition. Lower-income families that have been unemployed for three months or more would be given priority for assistance. Read more.
Even then, however, officials may want to maintain some level of surveillance testing in high-risk settings, like nursing homes, or of high-risk individuals, like travelers, she said.
Assessing our progress
Testing can help public health officials gauge whether efforts to end the pandemic are paying dividends.
“Do we want to know how well vaccines are working? We’re going to have to test,” said David O’Connor, a virologist at the University of Wisconsin, Madison. “How are we going to know whether the variants are more contagious? We’re going to have to test. How are we going to know if the vaccines are effectively controlling the variants? We’re going to have to test.”
Large screening programs may also help institutions assess the effectiveness of their risk-reduction strategies. If cases begin to rise, schools and offices may find they need to change their mask policies, enforce greater social distancing or boost their ventilation rates.
Testing might also help uncover worrisome case clusters, which can signal that a community has not yet reached herd immunity and might benefit from targeted a vaccination campaign.
Preventing the next pandemic
Many experts now believe that the coronavirus is unlikely to ever disappear completely. But even if the virus continues to circulate only at very low levels, it will be important to keep tabs on it.
“It becomes less about trying to interrupt the transmission of the disease and more to understand, Where is the virus?” Dr. Nuzzo said. “What are we missing? And, you know, what could be coming down the road?”
The virus will continue to mutate, and new genetic variants will emerge. Some level of continued testing, even years down the line, could help scientists catch worrisome variants early.
Tests aren’t perfect, of course, and can produce false negatives and positives. But they provide a critical window into the activity of a pathogen too small to see.
“We’re going to want to make sure that after people are vaccinated, it’s not going to bubble up in some other unpredictable way that’s going to put us back where we started,” Dr. O’Connor said.
Advertisement
