As patients returned to in-person, brick-and-mortar health care settings after the first wave of COVID-19 pandemic, they re-enter the health care system with heightened consumer expectations, according to the Beryl Institute – Ipsos Px Pulse report, Consumer Perspectives on Patient Experience in the U.S.
 Ipsos conducted the survey research among 1,028 U.S. adults between 23 September and 5 October 2020 — giving consumers many months of living in the context of the coronavirus.
Ipsos conducted the survey research among 1,028 U.S. adults between 23 September and 5 October 2020 — giving consumers many months of living in the context of the coronavirus.
This report is a must-read for people involved with patient and consumer health engagement in the U.S. and covers a range of issues. My focus in this Health Populi post is on the health consumer’s mindset in the age of COVID-19 and the re-shaped “enlightened” expectations of patients as the public health crisis persists longer than many people had anticipated.
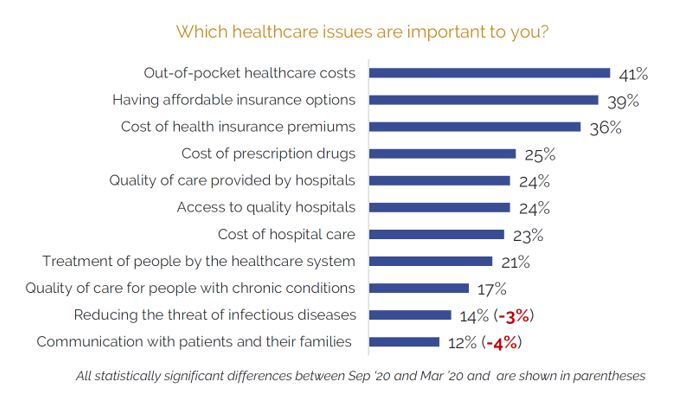
Regarding the most important health care issues U.S. consumers were facing in the autumn 2020, the first chart shows that many more people worried about costs — for out-of-pocket spending, affordable insurance, insurance premiums, and prescription drugs — than reducing the threat of infectious disease.
 Thinking about their health care experiences, consumers most-highly ranked having open access to their medical records and partnering for shared medical decisions with their health care providers as key to meaningful health engagement.
Thinking about their health care experiences, consumers most-highly ranked having open access to their medical records and partnering for shared medical decisions with their health care providers as key to meaningful health engagement.
To repeat, in other words: when it comes to judging the patient care experience, consumers put accessing their personal health information and partnering with providers on decisions as the top-two actions “reflecting meaningful participation in care experiences,” as the survey put it.
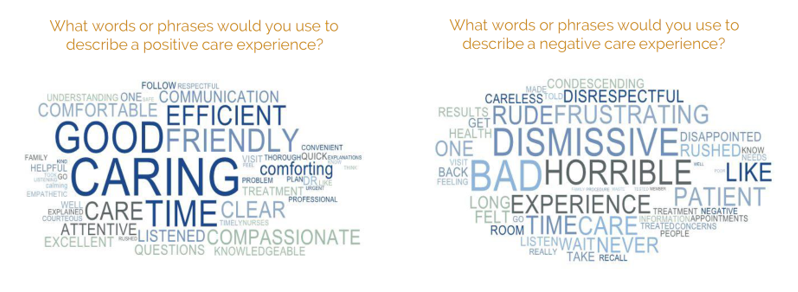
Looking at the wordle (the second graphic here), we see what words consumers used to describe a positive care experience compared with a negative one.
For a positive experience, consumers used words such as caring, good, time, friendly, efficient, attentive, listened, compassionate, clear, comfortable, and communication.
On the negative side of the experience ledger, people pointed to dismissive, bad, horrible, frustrating, time (in the “wasted” way), disrespectful, frustrating, and rude, among other less sanguine perceptions.
 Health Populi’s Hot Points: Both health care providers (hospitals, clinicians, allied professionals, et. al.) and consumers are stressed out by now, October 2020, in the wake of the coronavirus pandemic. I detailed the mental health impacts captured in the Stress in America 2020 survey yesterday here in Health Populi, which the American Psychological Association has tracked perennially since COVID-19 emerged in the U.S. early this year.
Health Populi’s Hot Points: Both health care providers (hospitals, clinicians, allied professionals, et. al.) and consumers are stressed out by now, October 2020, in the wake of the coronavirus pandemic. I detailed the mental health impacts captured in the Stress in America 2020 survey yesterday here in Health Populi, which the American Psychological Association has tracked perennially since COVID-19 emerged in the U.S. early this year.
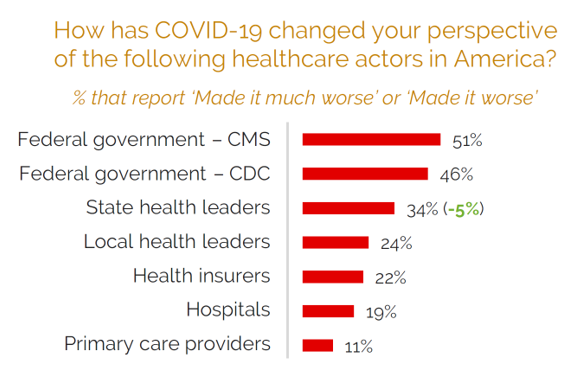
Some of the stress and anxiety felt across the U.S. has led to mis-trust in different health care stakeholder or institutional actors, shown in the third graphic taken from the Beryl Institute-Ipsos report.
The red bars indicate the percent of U.S. adults who said that COVID-19 negatively changed their perspective on, especially,
- 51% of people who pointed to the Centers for Medicare and Medicaid Services and
- 46% of Americans who cited the Centers for Disease Control (CDC).
 Note that the least-hurt health care actor during the pandemic in the eyes of consumer-trust were primary care providers, followed by hospitals, health plans, and local health leaders.
Note that the least-hurt health care actor during the pandemic in the eyes of consumer-trust were primary care providers, followed by hospitals, health plans, and local health leaders.
The results of the wordle picture above indicate that people are looking for empathy and understanding, which they find through clear instructions and information offered by their front-line providers — nurses and doctors, quantified in another question in the study.
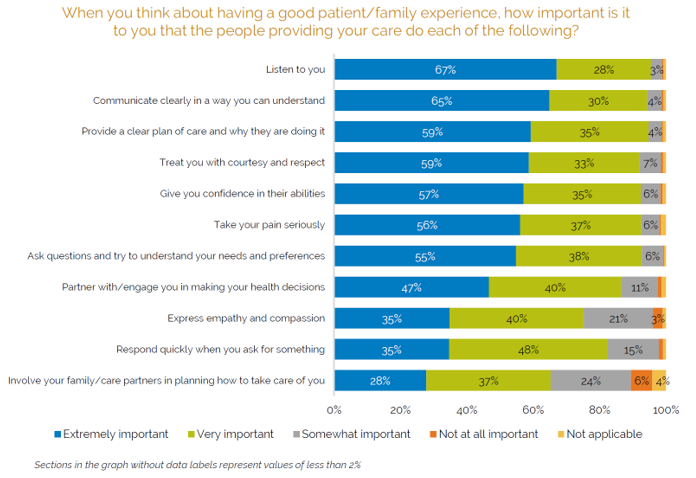
What emerges out of this important research is that a good health care experience is rooted in someone listening to “me,” communicating clearly to “me,” providing a plan of care that is for “me,” treating me with respect and courtesy, and giving me confidence in my ability to self-care, shown in the last chart.
Most people told Beryl and Ipsos that a negative experience with a healthcare organization would compel them to stop going to that provider or organization. Nearly one-half of consumers would tell another person about that experience, using the good old-fashioned viral tool of word-of-mouth communication.
COVID-19 has intensified consumers demand and need for positive, constructive, and empathetic patient experiences. These benefit both the patient herself in terms of outcomes and self-efficacy, but also provider organizations that need patients to return to normal patterns of care and workflow.
